Abstract
Background
Acute lymphoblastic leukemia (ALL) requires intensive systemic and intrathecal (IT) therapy for a prolonged period to prevent relapse [1, 2]. MRD negativity has been associated with long-term disease-free survival.[3] However, most published data are in patients treated in a clinical trial setting. Real-world data are lacking. We performed a retrospective cohort analysis of our database of ALL patients to determine the impact of MRD measurement on the pattern of relapse.[3-5]
Methods
We conducted a retrospective cohort analysis of patients with ALL treated at our institution between December 2001 and September 2015. We interrogated the database for patient and disease characteristics, treatment protocols, and outcomes. In all cases, MRD reported was obtained by way of multi-color flow cytometry on bone marrow biopsy samples. Data were stored in the RedCap database and simple, descriptive statistics were utilized for analysis. Chemotherapy consisted of standard regimens including E2993, Hyper-CVAD, the Vanderbilt ALL protocol, multiple pediatrics protocols, and multiple regimens not otherwise specified. [3-5]
Results
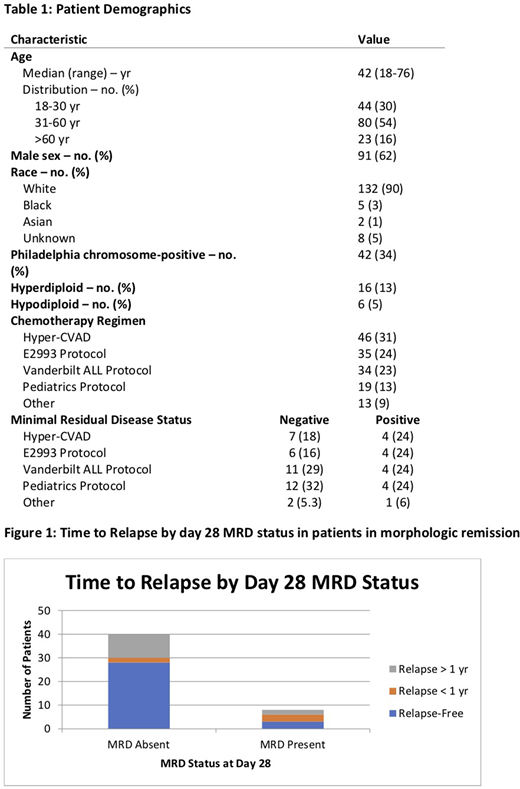
We identified 147 patients over the time period specified, consisting of 91 males and 56 females. The median age of the cohort was 42 years. The most common chemotherapy regimens used included Hyper-CVAD (31%), E2993 (24%), the Vanderbilt ALL protocol (23%) and pediatric protocols (19%). Among the patients in morphologic CR, 55 (37%) had MRD measured at day 28 (+/- 7 days). Of those patients, 38 (83%) were MRD-negative and 17 (13%) were MRD-positive. In the MRD-negative cohort, 2 (5.3%) relapses occurred within the first year while 8 (21%) ocured later. In the MRD-positive cohort, 3 (38%) relapsed within the first while 2 (12%) occurred later.
Discussion
Our results underscore the importance of early measurement of MRD in ALL patients in predicting early relapse. In those patients with no detectable MRD on flow cytometry of the bone marrow at day 28, only 5.3% relapsed within one year compared to 38% of those with detectable MRD. This difference is actually more pronounced than those observed in some clinical trials, validating early MRD measurement across treatment regimens in the real world setting. Notably, 2 patients with detectable MRD at day 28 were continued on the same protocol and did not relapse at 7-year follow-up. This suggests a potential role for serial MRD measurement in select, low-risk patients with MRD close to negative. Our study is limited as it is a retrospective analysis with a small sample size and at a single tertiary academic medical center which may diminish its applicability to other practice settings.
References
1. Bruggemann, M., et al., Clinical significance of minimal residual disease quantification in adult patients with standard-risk acute lymphoblastic leukemia. Blood, 2006. 107(3): p. 1116-23.
Cassaday, R.D., et al., Description and prognostic significance of the kinetics of minimal residual disease status in adults with acute lymphoblastic leukemia treated with HyperCVAD. Am J Hematol, 2018. 93(4): p. 546-552.
Mortuza, F.Y., et al., Minimal residual disease tests provide an independent predictor of clinical outcome in adult acute lymphoblastic leukemia. J Clin Oncol, 2002. 20(4): p. 1094-104.
Patel, B., et al., Minimal residual disease is a significant predictor of treatment failure in non T-lineage adult acute lymphoblastic leukaemia: final results of the international trial UKALL XII/ECOG2993. Br J Haematol, 2010. 148(1): p. 80-9.
Winter, S.S., et al., Safe integration of nelarabine into intensive chemotherapy in newly diagnosed T-cell acute lymphoblastic leukemia: Children's Oncology Group Study AALL0434. Pediatr Blood Cancer, 2015. 62(7): p. 1176-83.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal